It’s not easy, and most of us are not trained for it. You need to make decisions based on where you are….
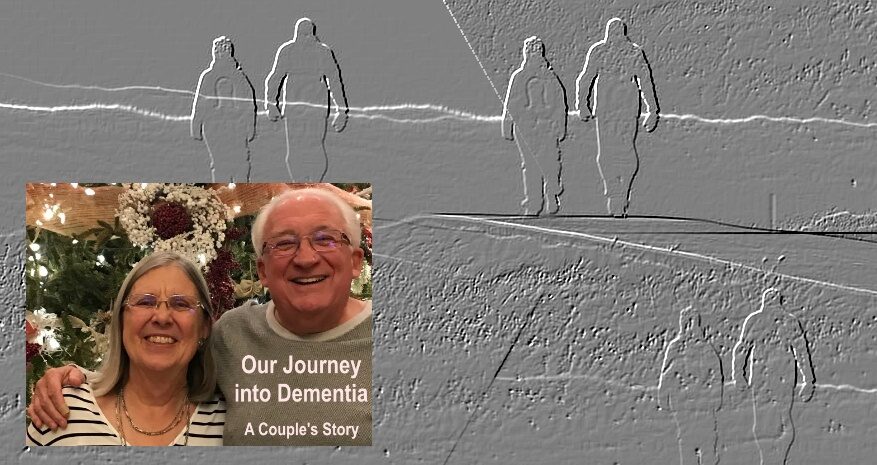
Seventh in a Series: This is part of an ongoing series about our family’s experience with dementia. There is no order to it, just observations, reflections and, I hope, some guidance for others on this journey or who may someday begin it. It is not intended as any sort of financial, medical or psychiatric advice. Just one family’s experience…
LAST TIME I said that as a care giver to my wife, as she lives with her dementia, I was confused about whether I was really giving care or acting as a guardian. I was not changing adult diapers, feeding her, helping her dress.
But, I think, I was caring for her and even though she no longer lives under the same roof with me, I still am.
Here’s what I have learned. Other care givers may have learned different things, had different experiences. As I have said before, no two cases of dementia are the same.
First, a “thank you” to our kids. Our son, Seth, lives 10 minutes away and has been a constant physical help. Our daughter, Andrea, lives in Europe but has come over and has been available on-line throughout.
I also have learned that caring is, in the end, an act of love expressed in small steps. On Aug. 10, 1968, I took a vow to be with Connie through for “better or worse.” You cannot accept the “better” then shrink from the “worse.”
I also have learned that unless you a nurse, psychiatrist, health aide you are not trained to give serious care. Even if you are in the health care field you may find it challenging to care for a loved one when you are wearing two hats.
Providing care to someone with dementia is not static. Situations change. At first, you will not be changing adult diapers or cleaning up messes. For the most part, you will find providing care just means being present. For instance, one of the earliest manifestations of my wife’s dementia, which we mistook for anxiety and depression, was an inability to deal with technology. She had taught on-line college courses, used legal sites as a lawyer and done email, Facebook and the like.
But, I began to notice that she was calling out to me more and more, sometimes several times an hour, to help her with what to me were almost sub-conscience types of tech activities. Obviously, this made it hard for me to settle into any routines. Before I realized what was going on, I didn’t always handle it well. I would get short with her. It was not until we finally realized what we were dealing with that I was able to show some patience.
As I’ve said in previous posts, she reached the point when she announced she no longer wanted to drive and I began doing all the driving, shopping, errands. That was followed by her giving up handling our financial affairs.
When we finally got a diagnosis of Frontal Temporal Degeneration and Primary Progressive Aphasia I began learning about dementia.
It’s a black hole that sucks you in and over time then closes itself behind you. I know that sounds awful, but what I mean is that as time goes by both the sufferer and care giver can become isolated and alone. As time went by, I became more and more concerned about leaving her alone. In her case, she became a bit of a recluse and would spend hours in bed. This was when I went to the grocery, or maybe sneaked down to the Y for a quick workout.
Even though I tried to keep up some kind of social calendar for her she became more and more nervous in crowds. We would go somewhere and very shortly after arriving, she would want to leave, so over time we did less and less of that. Notice I use the word “we” because as a care giver you are a part of your loved one and you often move, or don’t move, as one.
My own health began to decline. I worked out less, ate more. I gained weight. My sleep patterns became disrupted. I would often go back during the day and lie down with her rather than “doing” something. I did not leave for an extended periods of time because she had a fear that I would not come back, that something would happen to me.
There was a point when my kids noticed. I think I had declined more than I realized. One day my son just blurted it out. “Dad, I am afraid I am going to get a call that you’ve had a heart attack.”
At this point I still was not giving care in any kind of nursing sense. That is what differentiates dementia care from care for, say, a stroke or heart attack or cancer. But, if you decided to keep you loved one at home for as long as you can you may well find yourself changing adult diapers, dispensing medicines, helping them eat, bathe, dress. That is when the stress on you, the caregiver, will intensify.

For many people there are options. For example, a friend whose husband has dementia, and other conditions, has children who have been able to come for a few days and relieve her and she’s gone on solo trips to spas, for meditation. Others have hired home health care workers. Those are all good options.
If you choose to use home health care understand that private insurance, and Mediare, will not cover the actual presence of a home care worker. Insurance will cover “medical necessary” care if the person is providing purely medical services. But, for someone to simply be in the home with your loved one, it won’t. If you have a long-term health care policy it might, but you will want to be judicious about how you use those benefits. This link gives a good summary of insurance and home health care.
https://www.uhc.com/health-and-wellness/caregiver-resources/in-home-health-care
We did not opt for home care. Why not? We live in a two-bedroom apartment. If I had a home care worker come in, where would I really go? There is no spontaneity. What would I do? If I closed the door to our second bedroom, our office, could I write, do other things? In my wife’s case she would come and get me frequently when she needed something, often several times an area.
If we still lived in our previous house in a community where we (I) were more established the home health care worker certainly would have been a possibility. But in our apartment, it just didn’t seem like an option.
And, as I said above and in other posts, as time went by it became less about “care” and more about “doing as she either gave up or became unable to do certain things. A home health care worker is not part of a maid service.
Note: There is an excellent book on living with and loving someone with dementia by Dr. Pauline Boss. I found it very helpful. “Loving Someone Who Has Dementia: How to Find Hope while Coping with Stress and Grief.” Available online and at book stores)
As I read her book a couple of lessons from my past came back. One was from the college swim coach at Miami University in Ohio where I tried out for the swim team, failed but took every instructional swim course Raymond Ray taught. Coach Ray was kind man but he looked like the stereotypical cold-blue-eyed German officer in a World War II movie. I can remember clearly when he put what being a lifeguard meant in context.
“I don’t want any of you to ever be heroes. That’s not what this is about. The first duty of any lifeguard is to not become a second victim. Know when you cannot save another.”
Coach Ray also said, on our last day of class, something that seems to contradict that, but really does not.
“I will follow you. If I ever see that you lost a swimmer on your watch, I will come to you. I will make you look me in the eye and tell me what happened, why you did not save the life.”
What Coach Ray was saying there is a difference between making a decision that you cannot save a swimmer and simply failing to do so because you were afraid, or distracted, not doing your job. I think that applies to care giving.
Another lesson from my past, which I have written about before in other areas, comes from Cathy and Gary Hawk, friends and associates. They have a self-aware program called “Clarity.” In it they talk about the importance of “sacred selfishness.” For much of our lives we are taught to do for others. Others came first. It’s selfish to focus on our needs before we think of others.
Cathy and Gary don’t run away from that word “selfish.” They turn it around in a way most of us don’t often think about. The reality, they teach, is that if you are not in a good place, if you are not as healthy as you can be, then you are not going to be in any position to help others when they need it.
“Sacred Selfishness” is taking the time to keep yourself centered and health, both mentally and physically, however you choose to do that. If you do that regularly, then you will be more able to help those who count on you.
What Coach Ray and Cathy and Gary teach sounds easy enough, but it’s not. We had a saying down in East Texas that “when you are up to your butt in alligators, it’s hard to remember you went in to drain the swamp.” Care giving becomes consuming. You wonder if you can wander away for even a short while to take care of yourself.
But, you have to. Maybe it’s an hour at the Y. Maybe it’s going and sitting on a park bench while your loved one is asleep, or one of your kids is with them.
In the end, we came to that moment where I could not do that. I was sinking. My kids saw and we talked.
And here’s my final learning, or realization. No matter how you are providing care you will come to a time when maybe it won’t be enough and then it can get complicated, and tough. You reach the point where maybe your loved one needs more care you can give and you hope you can manage that. Maybe you reach the point where you realize your own mental and physical health are at risk. That’s when you make not just a gut-wrenching emotional decision, but one fraught with financial realities you never saw coming.
More on all that next time, and apologies if we start rambling a bit (what, we haven’t already?) but there are a lot of moving parts…
Rich Heiland, has been a reporter, editor, publisher/general manager at daily papers in Texas, Pennsylvania, Illinois, Ohio and New Hampshire. He was part of a Pulitzer Prize-winning team at the Xenia Daily (OH) Daily Gazette, a National Newspaper Association Columnist of the Year, and a recipient of the Molly Ivins First Amendment Award from the Walker County (TX) Democrat Club. He taught journalism at Western Illinois University and leadership and community development at Woodbury College in Vermont. Since 1995 he has operated an international consulting, public speaking and training business specializing in customer service, general management, leadership and staff development with major corporations, organizations, and government. Semi-retired, he and his wife live in West Chester, PA. He can be reached at [email protected].