When I heard there was a way I might be able to get more familiar with what my wife’s new world might be like, or might become, I was skeptical. But, I couldn’t say “no.”
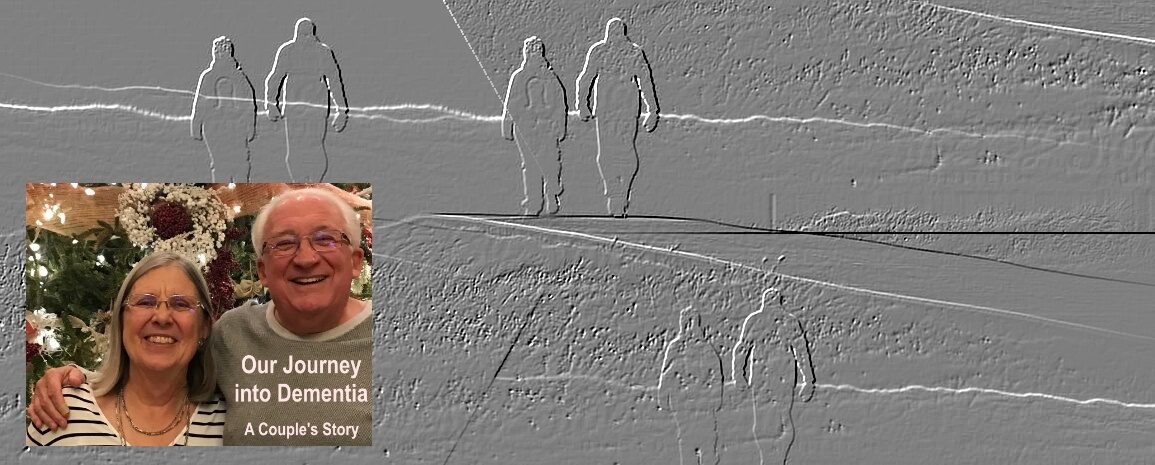
This is part of an ongoing series about our family’s experience with dementia. There is no order to it, just observations, reflections and, I hope, some guidance for others on this journey or who may someday begin it. It is not intended as any sort of financial, medical or psychiatric advice. Just one family’s experience…
FLASHING LIGHTS, SIRENS. Darkness. Confusion. An explosion.
No, I wasn’t somewhere in the Middle East. I was in a room at the care center where my wife lives in the memory care unit. I was at our monthly support group for families, and it wasn’t our usual setting. We weren’t around a big conference table. This meeting was designed to give us a feeling for what it’s like to have dementia. It was a designed simulation.

I admit I went into it with some skepticism. How on earth could anyone really know what it’s like to have dementia? And isn’t each sufferer unique? I still don’t think it’s possible to exactly replicate in someone who does not have dementia what it’s like. However, it is possible to create a situation which may mimic what someone with dementia experiences.
The simulation is based on a couple of different levels of study. The first is based on observation. We have years, decades, of observation both in terms of formal studies and what those caring for dementia-sufferers have seen. The outward signs of dementia have been well-noted, and there have been medical and psychological studies on what causes those outward signs.
Additionally, there have been interviews with dementia patients where they have been able, up to a point, to describe their feelings.
The creators of the simulation took all that and created an “experience.” It’s designed to show all the confusion, the frustration, the fears, the distractions, the physical challenges of living with dementia. The simulations were designed primarily with the staffs of care centers in mind. These are the people who deal with the many manifestations of dementia daily. But they also are available for families of those with dementia and that’s how I came to be in that dark room.
THE ROOM WAS set up with a table and chairs. On that table were a sweater as well as a pitcher of water and glass. Or at least, so I was told. It was dark and I never saw them. We were asked to put on heavy work gloves, as well as headphones. We put on glasses that had small holes in the center, narrowing our vision.
When I put on the headphones, I could hear multiple conversations going on. It was like being in a small room with 20 people, all of them saying some different to the point any single conversation was lost. After I put them on the monitor began reading something to me. I tried to concentrate but all I could not hear her over the noise in the headphones. I could see her lips moving but whatever she was saying was lost to me.
After she said whatever she said, she led me in the room and positioned me. I stood there. I stared at the wall, hearing all the conversations. Strobe lights flashed, other lights came and went. There were sounds. Police and fire sirens, alarms, an explosion. I stood there for something like eight minutes. I didn’t move.
At the end of the time they came and got me. That was it. When I got back to the waiting area I saw the monitor’s notes. Under “strange behaviors” it said “He never moved after he entered the room.” I asked her why that was “strange.”
“Because. You didn’t do any of the tasks I gave you,” she said. What tasks? As it turned out I was supposed to move around the room. I was supposed to try to pour water from the picture, to get the sweater on, both while wearing heavy gloves and dealing with all the flashing lights, sirens, explosions and conversations in my ears.
That was what she had told me when I saw her lips moving but didn’t hear any words.
OK. SO, WHAT was I supposed to gather from all this? I talked to some of my group mates to see what they had experienced. Most of them had tried the tasks. Here is what we got out of it:
- Dementia messes with the mind. Things get short-circuited. Our loved ones are seeing, hearing, feeling things inside their world we don’t see, hear or feel so we can’t expect them to act as we would, or as we once would have expected them to.
- There can be physical manifestations with dementia. Simple tasks become hard. Coordination is dicey. Things like buttoning a shirt, managing a TV remote at some point may escape a dementia patient. I thought of my wife trying her best to write in her journal but taking forever to scrawl a few words.
- There also can be feelings of paranoia, of fear, panic. Most of us who were in that room, dealing with everything coming at us, at some point felt confusion, disorientation. I made a connection with a man in the memory unit who would get very agitated at noise. I thought of the woman who constantly cried for help and thought the staff was ignoring her.
- Sense of time can change. I had no idea how long I was in the room. I was distracted. I thought of the woman in the unit who always asks “can I have breakfast now?” only to be told “You had breakfast and lunch. In two hours we will have dinner.”
- I think if there was one thing we all got out of it, it was the need for patience. I admit to being an impatient person. I always have been. I like to move, to do. I can sit quietly but only when I don’t feel like there is a need to be doing something. Put me on a path and I want to walk it. Now. I know I’ve become frustrated with Connie when it takes her so long to do what she used to do in seconds or minutes. I am not being fair in my impatience.
I still don’t think what it feels like to live inside dementia can ever be truly simulated. But I did come away from this experience thinking that at least there is a tool that can give you some idea of all the different sensations that can be inside someone with dementia.
I think any caregivers, any loved ones of a dementia patients, would benefit from this experience. I am guessing if you ask your care unit, or professionals you are working with about this kind of experience, they can direct you to it. In our case the company involved is “Second Wind Dreams.” There are others. Check it out.
Rich Heiland, has been a reporter, editor, publisher/general manager at daily papers in Texas, Pennsylvania, Illinois, Ohio and New Hampshire. He was part of a Pulitzer Prize-winning team at the Xenia Daily (OH) Daily Gazette, a National Newspaper Association Columnist of the Year. Since 1995 he has operated an international consulting, public speaking and training business specializing in customer service, general management, leadership and staff development with major corporations, organizations, and government. Semi-retired, he and his wife, Connie, live in West Chester, PA. He can be reached at [email protected].

Thank you so much for sharing! Lauren sent me your article and it made my day. Your insights are so great and I’ll definitely be sharing with others!
Allie Mazza (the person who led the VDT you went through!)